Although pediatric patients represent only 1% of all new cancers diagnosed in the US, approximately 1 in 285 children in the US will be diagnosed with the disease before the age of 20. Cancer is the second leading cause of death (following accidents) in children ages 5-14.1 Unlike many adult cases, the causes of cancer in most children is unknown.
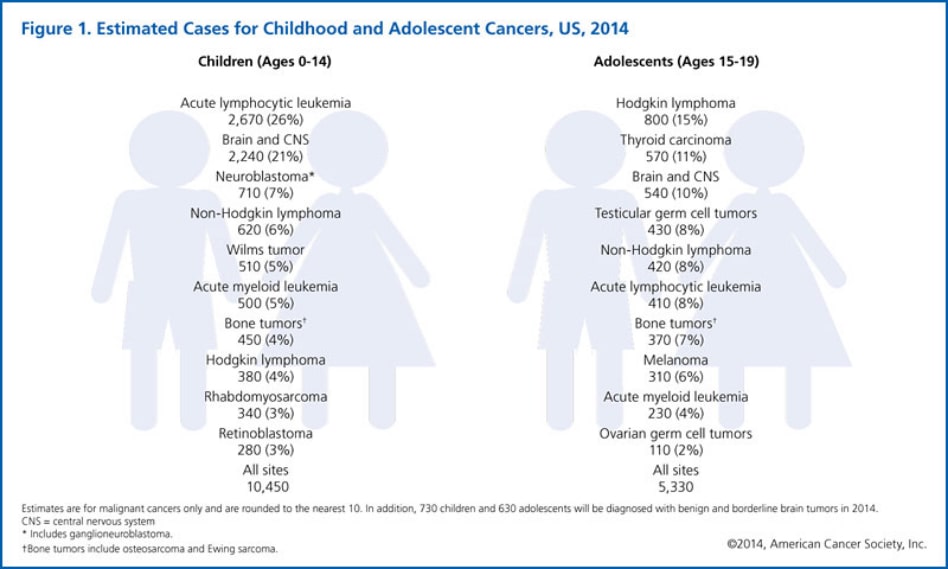
Cancer in children can affect almost all areas of the body, but many occur in tissues that are growing or developing rapidly, including bone and bone marrow, the brain, soft tissues like muscle and blood vessels, and developing organs like the kidneys. The types of cancers that develop in children and adolescents differ from those that develop in adults. The predominant types of pediatric cancers (ages 0-19) are leukemia (26%), cancers of the brain and central nervous system (CNS) (18%), and lymphoma (14%).
Many childhood tumors tend to spread early in the course of disease, making chemotherapy important in their management. With the exception of leukemia, the majority of childhood cancers are treated with surgery and/or radiation. When it can be performed without important cosmetic or functional compromise, the preferred treatment for local tumors is surgery. Radiation therapy is often used in the treatment of rhabdomyosarcomas, non-rhabdomyosarcoma soft tissue sarcomas, Ewing tumors, osteosarcoma, medulloblastomas, ependymomas, germ cell tumors in the brain, retinoblastoma, advanced Wilm’s tumor, neuroblastoma, and Hodgkin’s disease. Radiation therapy is a powerful tool that increases the likelihood of successful cancer treatment, but may also cause side effects. The nature and severity of side effects depend on the tumor’s location and type, its extent and radiation dose. Side effects may occur at any time after treatment, even 50 years later. Growing tissue in children is particularly susceptible to radiation therapy. Brain tissue in the very young can be damaged by very low doses of radiation and growing muscle and bone may also show signs of reduced potential growth following low doses of radiation. For this reason, when using radiation it is critical to avoid as much normal tissue in children as possible. In addition, radiation has the potential risk of causing another tumor many years after treatment. These can be benign or malignant. The smaller the volume of tissue treated, the less the risk.
Because of the young age and high curability of many childhood cancers, treatment outcomes are important areas of concern. Radiation therapy can cure many of the solid tumors in children that cannot be easily removed with surgery.
Treatment outcomes following radiotherapy are important for patients of all ages. However, due to the unique sensitivity of developing organs and the high curability of many childhood cancers, the undesirable effects of radiotherapy have been the subject of many recent studies involving conventional radiation in children.
Because pediatric cancers are rare, most experts strongly recommend that they be treated at medical centers with specialization in childhood cancer by multidisciplinary teams including pediatric radiation oncologists, pediatric neurosurgeons, pediatric oncologists, and other specialists. At pediatric cancer centers, treatment protocols are available for most types of cancer that occur in children and adolescents, and the opportunity to participate in clinical trials is offered to most patients and their families. The University of Florida belongs to the Children’s Oncology Group (COG), a National Cancer Institute-supported clinical trials group. COG doctors care for more than 90% of US children and adolescents diagnosed with cancer. All the pediatric radiation oncologists at the University of Florida Health Proton Therapy Institute are members of COG and many hold leadership positions.
1 Murphy SL, Xu J, Kochanek KD. Deaths: Final data for 2010. National vital statistics reports; vol 61 no 4. Hyattsville, MD: National Center for Health Statistics, 2013.
Types of pediatric cancer treated with proton therapy include:

